Rectal Prolapse
The Complete Guide to Rectal Prolapse: Prevention, Diagnosis, and Recovery
Rectal prolapse is undoubtedly one of them. It's a condition that many are hesitant to discuss, but understanding it is crucial for prevention, timely diagnosis, and effective recovery. Let's shed some light on this often-misunderstood issue.
What is Rectal Prolapse? The Meaning Behind the Medical Term
At its core, rectal prolapse meaning refers to a condition where the rectum (the last section of the large intestine, just before the anus) turns inside out and slides out through the anal opening. Think of it like a sock that's been turned inside out and then pushed out through an opening.
It's important to distinguish this from hemorrhoids, which are swollen blood vessels. While both can cause lumps around the anus, rectal prolapse involves the actual lining or full wall of the rectum.
Types of Rectal Prolapse
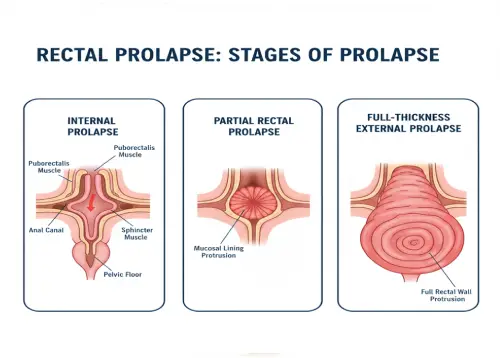
Not all prolapses are the same. There are generally three types:
-
1. Partial Rectal Prolapse (Mucosal Prolapse) :
- This is where only the innermost lining of the rectum protrudes. It usually involves a smaller protrusion, often only visible during bowel movements. This is a key term to understand as it represents a less severe form compared to a full prolapse.
-
2. Complete Rectal Prolapse :
- Here, the entire wall of the rectum, not just the lining, telescopes out through the anus. This is more noticeable and can occur with straining, coughing, or even just standing.
-
3. Internal Rectal Prolapse (Intussusception) :
- In this case, the rectum folds in on itself but doesn't protrude outside the body. While not visible externally, it can cause symptoms like incomplete evacuation and a feeling of blockage.
What Causes a Rectal Prolapse?
While the exact cause isn't always clear, several factors contribute to the weakening of the muscles and ligaments that hold the rectum in place:
-
• Chronic Straining :
- Long-term constipation and excessive straining during bowel movements are major culprits.
-
• Weak Pelvic Floor Muscles :
- Childbirth, aging, and certain neurological conditions can weaken the muscles and ligaments that support the rectum. Women, especially older women who have had multiple vaginal deliveries, are more commonly affected.
-
• Previous Surgery :
- Some abdominal or pelvic surgeries can increase the risk.
-
• Neurological Conditions :
- Conditions like spinal cord injury or multiple sclerosis can affect nerve function to the pelvic floor.
-
• Cystic Fibrosis :
- In children, this genetic condition can sometimes be linked to rectal prolapse.
Recognizing the Symptoms
The most obvious symptom is seeing or feeling a reddish mass protruding from the anus, especially during or after a bowel movement. Other symptoms can include:
- Difficulty controlling bowel movements (fecal incontinence): This can range from leakage of mucus to loss of solid stool.
- A feeling of incomplete bowel evacuation.
- Rectal bleeding or discharge.
- Rectal pain or discomfort.
- The need to manually push the prolapse back in.
If you suspect you have a prolapsed rectum, it's vital to see a doctor. The NHS (National Health Service in the UK) strongly advises seeking medical attention for any new rectal protrusion or bleeding. Understanding rectal prolapse NHS guidelines can provide further resources and guidance if you're in the UK.
Diagnosis: What to Expect
Diagnosing rectal prolapse typically involves:
-
• Physical Examination :
- Your doctor will likely ask you to "strain" as if having a bowel movement while lying on your side or sitting on a commode. This helps them see the prolapse if it's present.
-
• Defecography :
- This is a special X-ray or MRI study that allows doctors to visualize the rectum and pelvic floor muscles during a bowel movement.
-
• Colonoscopy or Sigmoidoscopy :
- These procedures use a flexible tube with a camera to examine the inside of the colon and rectum, ruling out other conditions.
Treatment and Recovery: A Path Forward
The good news is that rectal prolapse is treatable. The primary treatment for a full or complete prolapse is almost always surgery
-
Surgical Options :
- ✅ Abdominal Repair : This approach involves surgery through the abdomen. The surgeon can either pull the rectum up and attach it to the sacrum (rectopexy) or remove a section of the colon and then perform a rectopexy.
- ✅ Perineal Repair: This approach involves surgery through the area between the anus and genitals. While it has a lower risk of complications for some, the recurrence rate can be slightly higher than abdominal repairs. Your surgeon will discuss which option is best for your individual situation.
-
Non-Surgical Management (for partial prolapse or to improve symptoms) :
- ✅ Dietary changes: High-fiber foods, plenty of fluids, and stool softeners can help prevent straining and constipation.
- ✅ Pelvic floor exercises: Strengthening these muscles can sometimes help with partial rectal prolapse and improve continence.
Recovery from surgery typically involves managing pain, avoiding straining, and gradually increasing activity. Most people find significant relief from their symptoms and a much-improved quality of life after successful treatment. Post-operative care often includes continued attention to bowel habits to prevent recurrence.
Prevention: Taking Proactive Steps
While not always preventable, you can significantly reduce your risk of rectal prolapse by:
- Avoiding Constipation: Eat a high-fiber diet, drink plenty of water, and consider fiber supplements if needed.
- Don't Strain: If you feel the urge, go. Don't hold it in, and avoid prolonged sitting on the toilet.
- Manage Chronic Cough: If you have a persistent cough, seek treatment to reduce repeated abdominal pressure.
- Strengthen Your Pelvic Floor: Especially for women, regular pelvic floor exercises can be highly beneficial.
